More Details on POS Plans
October 21, 2016As we’d shared in a previous flash, we’re offering Medicare Advantage point of service (POS) plans instead of preferred provider organization (PPO) plans for 2017.
Our new POS plans were designed to mimic the PPO, so members’ costs are determined by where they get their care. Like a PPO, POS plans provide out-of-network coverage, but members will pay less when they get care in-network.
The biggest difference between a PPO and a POS is that members must choose a primary care provider (PCP) on a POS plan. Their PCP will direct their care. While we encourage members to work through their PCP to manage referrals to other providers, it will be up to the PCP and the specialist to decide on the referral process.
Current PPO members must enroll in an HMO or POS plan to keep their coverage with Health Alliance Medicare. Learn more about the steps we’ve taken to help these members transition.
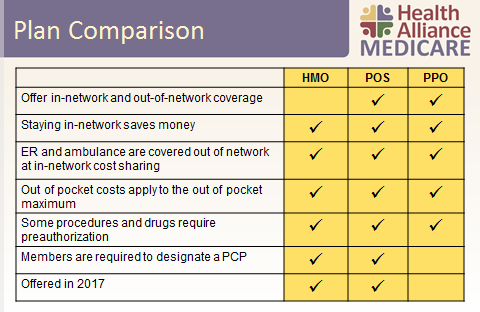
This chart helps break down how a POS plan is a blend of a health maintenance organization (HMO) and PPO: